Device can be configured to deliver lifesaving medication for hypoglycemia, anaphylaxis, and other conditions
Developed by engineers at MIT, a novel implantable device offers a potential life-saving solution for individuals prone to medical emergencies, such as those with Type 1 diabetes at risk of severe hypoglycemia and those with allergies prone to anaphylaxis.
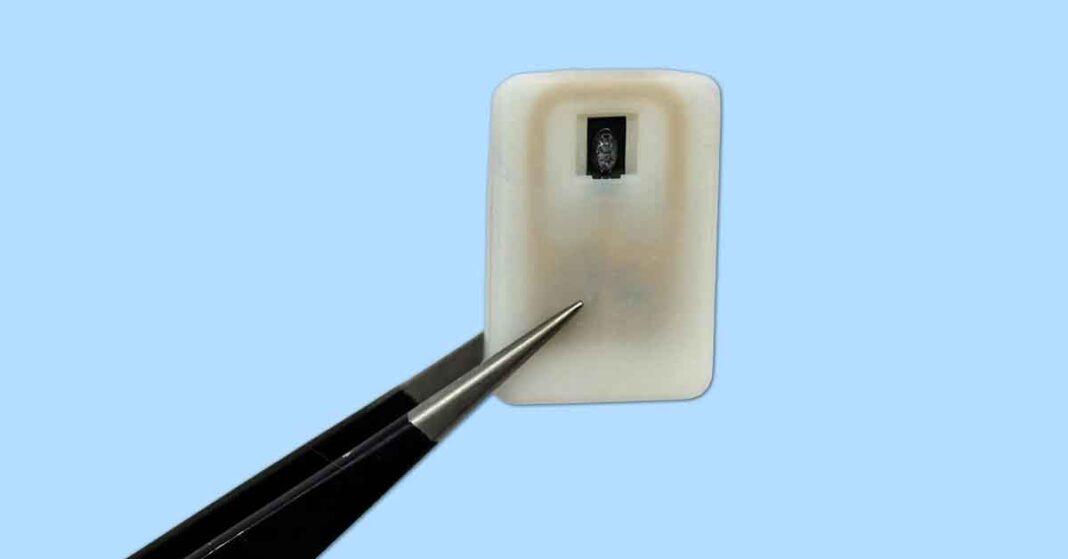
This compact device, roughly the size of a quarter, is designed to be placed under the skin and contains a reservoir of powdered medication. Initially, the primary focus of its development was to store and automatically release glucagon, a hormone critical for raising dangerously low blood sugar levels, thereby preventing the severe complications associated with hypoglycemia, such as disorientation, seizures, and even death.
The device’s innovative mechanism relies on a 3D-printed polymer reservoir sealed with a shape-memory alloy. This nickel-titanium alloy is engineered to change form and release its contents when heated to 40 degrees Celsius. The powdered drug formulation ensures stability over extended periods, a crucial advantage for peptide-based medications like glucagon, which typically degrade rapidly in liquid form. The system is equipped with an antenna that responds to specific radio frequency signals, allowing for both manual activation and automatic triggering via wireless signals from external sensors, such as continuous glucose monitors.
Crucially, the research extends beyond diabetes management, demonstrating the device’s versatility for other critical medical interventions. The MIT team successfully adapted the technology to deliver emergency doses of epinephrine. This capability is significant for treating anaphylaxis, a severe and potentially life-threatening allergic reaction to a food, drug, insect venom or environmental substance. The ability to automatically or wirelessly trigger epinephrine release could provide a vital, rapid response to anaphylactic shock, which often requires immediate medication to prevent severe symptoms and fatal outcomes.
The potential for anaphylaxis management is particularly impactful because epinephrine auto-injectors need to be carried by individuals at risk and administered promptly, which can be challenging during an acute allergic reaction, especially for children or in situations where the individual is incapacitated. An implanted device that can deliver epinephrine automatically upon sensor input or with minimal intervention offers a significant improvement in emergency preparedness and patient safety, reducing the dependence on manual injection during a high-stress event.
In trials with diabetic mice, the device effectively prevented hypoglycemia by releasing glucagon, with blood sugar levels stabilizing within 10 minutes. Similarly, when tested with powdered epinephrine, the device led to elevated epinephrine levels and increased heart rates within the same timeframe, demonstrating its efficacy for rapid drug delivery. The researchers observed that the device remained functional even with the formation of scar tissue, a common issue with implanted medical devices, suggesting long-term viability.
Looking ahead, the researchers aim to extend the device’s implant duration to at least a year and plan for further animal studies, with clinical trials anticipated within the next three years. This groundbreaking technology, initially conceived for diabetes care, holds immense promise for revolutionizing emergency medicine by providing a dependable, readily available, and potentially automated method for delivering life-saving medications, particularly for conditions like anaphylaxis where timely intervention is paramount.