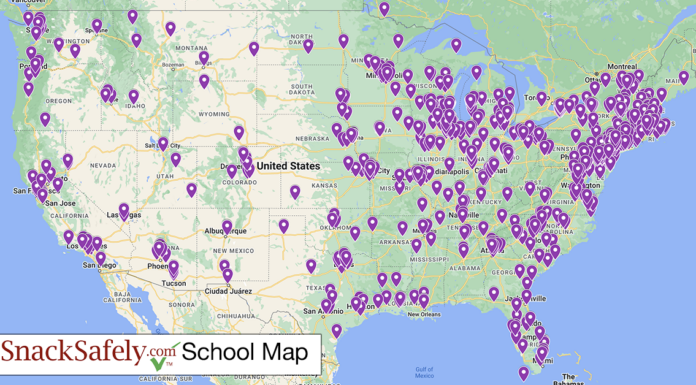
Established in 2011, SnackSafely.com provides straightforward, actionable information to help improve the lives of the estimated 32 million people in the US suffering with food allergies.
We strive to eliminate anaphylaxis by leveraging our on-line properties to educate, advocate, and connect the allergic community with products and services that help toward achieving this goal.
Our blog covers topics of interest to the food allergy community including news reports; ongoing research, clinical studies, trials and progress toward treatment and cure; general advocacy; and advice regarding food safety and school policies.
Please see our Terms of Service and Privacy Policy.
Copyright ©2011-2024 SnackSafely.com, Inc — All rights reserved