Ticks are spreading across the US with a vengeance as a result of the relatively warm, wet winter. Along with a host of horrific diseases, ticks are responsible for spreading alpha-gal syndrome, an allergy to a complex disaccharide sugar found in mammalian (red) meat.
The danger has become so prevalent that the US military is warning service members to protect themselves.
Here follows an advisory posted to the US Army website, which provides information disseminated by the Defense Health Agency Public Health. We also offer an alpha-gal Q&A answers all your questions including how to protect yourself.
Military Health Experts Warn about Potentially Life-Threatening Meat Allergy from Tick Bite
By V. Hauschild, MPH, Defense Health Agency Public Health
The Centers for Disease Control and Prevention estimates that more than 500,000 people in the U.S. have a serious allergic condition called alpha-gal syndrome, or AGS, also known as the red-meat allergy or tick-bite meat allergy.
If AGS is not diagnosed and managed, patients may suffer with painful mystery symptoms for years. In severe cases, AGS can cause anaphylaxis, a life-threatening allergic reaction. Data show that cases of AGS are rising in the U.S.
What is Alpha-gal Syndrome?
AGS is a tick bite-related condition that causes allergic reactions from eating red meat, including beef, pork, rabbit, lamb, and venison. Some AGS sufferers also develop allergies to dairy and to meat byproducts such as meat broths, gelatins, and certain pharmaceuticals, including some capsule coatings. Poultry and fish products are not linked to AGS.
AGS is named after the alpha-gal antigen that enters a tick’s saliva when it feeds on a source mammal. This antigen can then be transmitted to humans through a tick bite. The human body sees the antigen as a foreign invader and produces antibodies that trigger the immune system’s allergic response. When an infected person later consumes, for example, a steak or a gelatin-coated capsule that contains the alpha-gal antigen, they may have an allergic reaction. For reasons not completely understood, this does not happen to everyone.
Who can Get Alpha-gal Syndrome?
Evidence suggests that AGS is primarily associated with the bite of the lone star tick in the U.S., but other tick species have been associated with the development of AGS in other countries. Most cases have been reported in adults, though any age group can develop AGS. Aside from tick bites, no other risk factor is known.
Is Alpha-gal Syndrome New? Where is it From?
AGS was discovered over 15 years ago when scientists discovered that many anaphylactic allergy emergency cases were occurring in people who had consumed red meats or taken certain cancer drugs and also had a prior lone star tick bite. The link was confirmed when locations of cancer drug-related allergy cases overlapped with the primary habitats of the lone star tick in the Southeast U.S.
According to CDC surveillance, AGS cases in the U.S. steadily increased from 2019 to 2022. Highest numbers were in Suffolk County, New York, followed by counties in Virginia and Kentucky, all lone star tick habitats. While some cases occurred in areas outside known lone star tick habitats, other states with high numbers of AGS cases were lone star tick habitats in the South and Central U.S.
The CDC recognized the emerging significance of AGS by establishing a unique AGS medical code, Z91.014, in January 2022. However, CDC reported in a July 2023 Health Advisory that many health care providers still had not heard of AGS or would not recognize if a patient’s symptoms were related to AGS. Since AGS diagnoses do not require CDC notification, the true number of cases is unknown.
U.S. Army Lt. Col. Scott Robinson, a preventive medicine clinician now working for Defense Health Agency Public Health, has recognized that the military family is not immune to AGS.
“A military study looking for AGS in 3,000 service members’ blood serum samples saved between 2002 and 2007 found 180 positive cases,” said Robinson. “So, AGS was occurring in military personnel over two decades ago. But since it’s not a reportable disease, we have not been tracking it.”
AGS in the Military Population
To provide more current military evidence, Robinson teamed up with Kiara Scatliffe-Carrion, a senior DHA-PH epidemiologist, to analyze all service military hospital and clinic records from January 2022 through September 2023.
Robinson and Scatliffe-Carrion found the number of AGS diagnoses is growing in the military. Their analysis found 1,080 individuals with AGS diagnosis, and case numbers were increasing in same-month comparisons between years.
Almost half of military AGS cases were from the Army, though most were not soldiers, but family members, retirees, and others. Two-thirds of the cases were diagnosed at locations in the Southern U.S. Cases were also diagnosed in the Northeast and Central U.S., which corresponded with CDC’s AGS surveillance findings.
What are Symptoms of Alpha-gal Syndrome?
“AGS can have a range of typical allergic symptoms that occur after exposure to the allergen, said Robinson. “But unlike other allergies, symptoms are not immediate and usually don’t appear for two to six hours.”
Symptoms may include:
- Hives or itchy rash
- Nausea or vomiting
- Heartburn or indigestion, or even severe stomach pain
- Diarrhea
- Cough
- Shortness of breath or difficulty breathing (in extreme cases anaphylaxis)
- Drop in blood pressure
- Swelling of the lips, throat, tongue or eyelids
- Dizziness or faintness
“The response is most often after consumption of a meat, such as a steak or burger, but could also be another product containing alpha-gal (for example, gelatin-coated medications),” said Robinson. “The delay in symptoms showing up may be why an allergic condition is not considered by many doctors or their patients.”
A common scenario is someone who wakes up in the middle of the night with itching or hives, then develops gastrointestinal pain, abdominal cramping, and diarrhea. The symptoms may be severe, and then pass but reoccur for years before the cause is discovered.
Robinson explains that AGS can only be confirmed with a specific laboratory test of blood serum that looks for the antibodies to alpha-gal, known as an AGS-specific immunoglobulin, or AGS IgE test. This allergen-specific test is not performed unless AGS is suspected.
“Most often, patients will see a general health care provider who does not specialize in allergies,” said Robinson. “These doctors may examine patients and even conduct basic blood testing and find nothing wrong. Since these providers aren’t thinking of AGS, a diagnosis can be delayed for months or possibly years.”
What Should You Do?
Robinson highlights the following actions:
1. Prevention: How can I avoid getting AGS?
Ticks can transmit AGS as well as many other serious diseases such as Lyme disease, so avoiding tick bites, or at least quickly identifying ticks on you and removing them before they can transmit a disease, should be everyone’s goal.
The Military Health System’s tick-borne illness website offers tips for avoiding tick-borne diseases, including:
- Avoid tick habitats. Avoid tall grasses, brushy and wooded areas; stay in the middle of trails. Take steps to prevent ticks on your pets and in your yard.
- Dress to protect yourself. Wear hats, long sleeves, and pants tucked into socks or boots. Wear light colors to help spot ticks. Use permethrin to treat clothing and gear or buy pre-treated wear (permethrin is not to be put directly on skin).
- Check yourself. Once inside, do a tick check of clothing, gear, and your body (in and around hair and ears, under the arms, inside the belly button, around the waist, between the legs, back of the knees). Shower right away, as the flow of water can help dislodge and remove ticks that haven’t latched on yet.
- Remove ticks quickly. Immediately remove any tick found embedded. Use tweezers. Do not use heat, nail polish, or petroleum jelly to try to make a tick detach.
- Submit a tick removed from a human for testing. The Department of Defense MilTICK program allows active duty service members, DOD beneficiaries, contractors, and civilians, to submit their ticks for free testing. Although MilTICK doesn’t currently test for tick AGS, the tick submitted for testing could be a carrier for another condition, such as Lyme disease.
2. Early diagnosis: How do I know if I have AGS?
Doctors and patients should be familiar with AGS and consider the possibility of this condition, particularly if there is known or possible past tick exposure. While many tick-borne diseases can have similar signs and symptoms, such as fever, chills, or a rash, AGS symptoms may occur long after a tick bite.
A health care provider will need to review your history of symptoms and any past tick exposure and conduct the alpha-gal antibodies blood test. An allergy skin test may also be performed. The provider may refer you to an allergist or immunologist.
3. Medical management: What should I do if I have AGS?
AGS should be managed under the care of an allergist or other health care provider. Proper dietary changes allow those who have it to live normal lives, though medication for allergic reactions may be advised under the care of a provider. It’s important to be aware of antigen sources that might trigger an allergic response. Tips for managing AGS include:
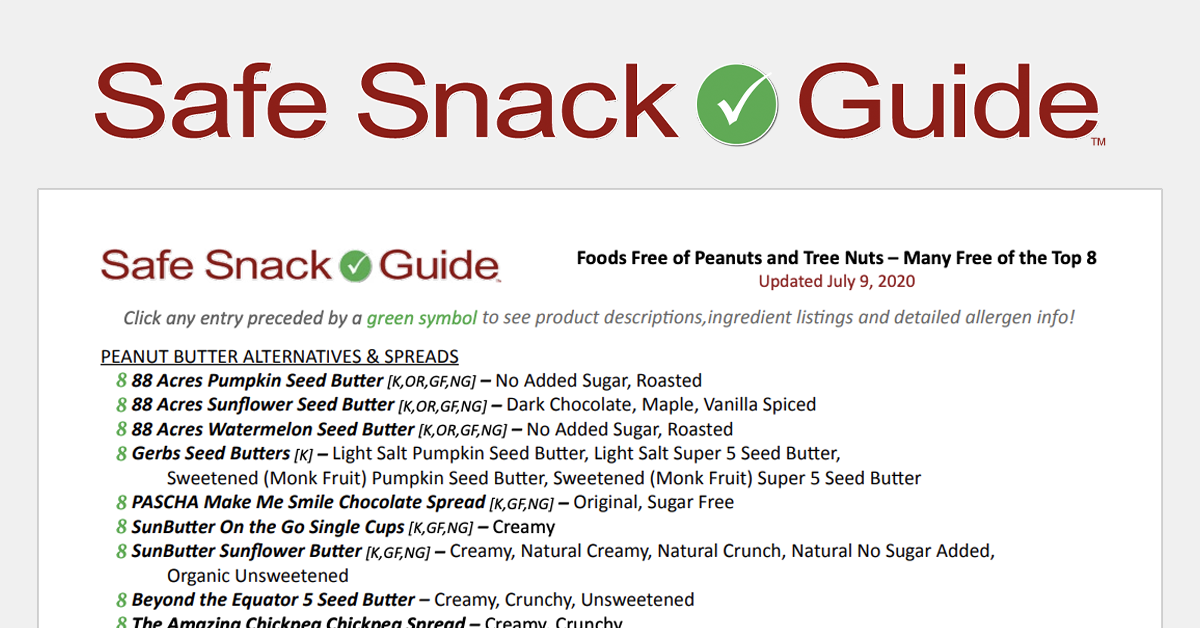
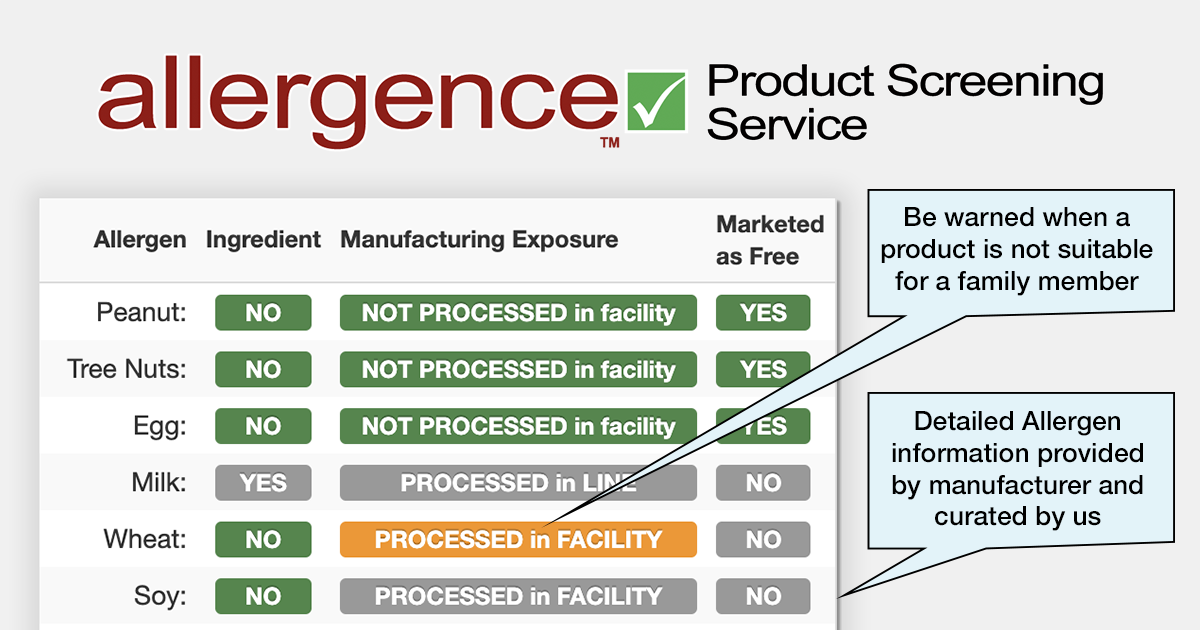
- Avoid products that can cause you to have an allergic reaction, and read food labels carefully.
- Most doctors recommend patients with AGS stop eating mammalian meat.
- Depending on the severity of a patient’s allergic reaction, doctors may also suggest that AGS patients avoid other foods and ingredients which may contain alpha-gal such as milk products and gelatin. Find out more about products that you may need to avoid here.
- Although very rare, some people with severe AGS may react to ingredients in certain vaccines or medications. Talk to your health care provider before taking a new medication or receiving a vaccine.
- Prevent additional tick bites. New tick bites may reactivate your allergic reactions to alpha-gal. It is possible that your AGS symptoms will lessen or go away completely after a couple years if you receive no additional tick bites.
Robinson and Scatliffe-Carrion recognize that as AGS becomes more recognized by doctors, the number of cases diagnosed may continue to increase.
“Previously unrecognized cases are hopefully going to be identified by health care providers so patients can finally put an end to the mystery symptoms and manage their disease,” said Robinson. “But the ultimate goal is for people to take better precautions against tick bites, which will help reduce the disease occurrence.”
The Defense Health Agency supports our Nation by improving health and building readiness–making extraordinary experiences ordinary and exceptional outcomes routine.
NOTE: The mention of any non-federal entity and/or its products is for informational purposes only, and not to be construed or interpreted, in any manner, as federal endorsement of that non-federal entity or its products.