Researchers in France have identified a cellular mechanism that controls the release of inflammatory factors that cause severe allergic reactions. The discovery could pave the way for new therapies to combat or prevent anaphylaxis.
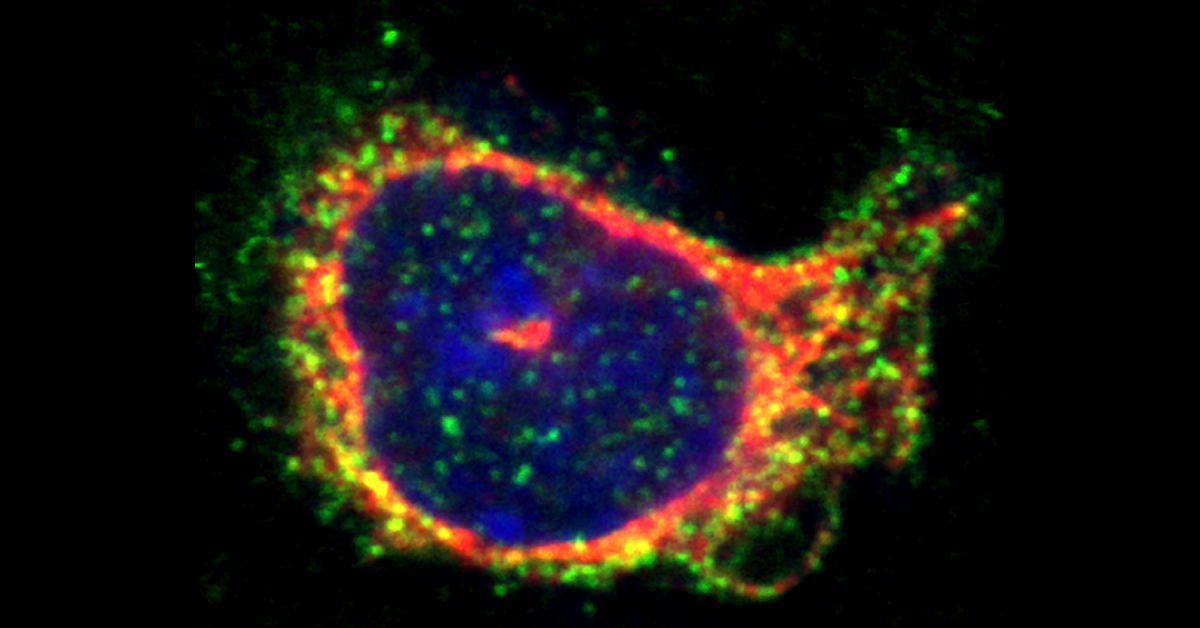
To understand how this mechanism works, we start by looking at the mast cell found in tissues throughout the body that help fend off parasitic infections. These cells work by releasing histamine and other inflammation-causing compounds when the body is attacked.
Unfortunately, allergens can also trigger this release, causing facial swelling, difficulty breathing, and a sudden drop in blood pressure that can potentially render the victim unconscious. The only treatment for such life-threatening reactions – called anaphylaxis – is epinephrine (aka adrenaline) administered via injection.
The researchers investigated the role of kinesin-1, a motor protein that transports compounds from the mast cell interior to the outer membrane where they are released. They created mice whose mast cells lacked a key subunit of kinesin-1 called Kif5b. These mice proved much less sensitive to allergen-induced anaphylaxis because the quantity of the inflammatory compounds transported to the outer membrane upon mast cell activation was greatly reduced.
“The fact that mice lacking Kif5b in their mast cells exhibited very low levels of passive, systemic anaphylaxis suggests that kinesin-1 could be a valuable new therapeutic target for controlling allergic reactions,” Gaël Ménasché, one of the lead researchers said.