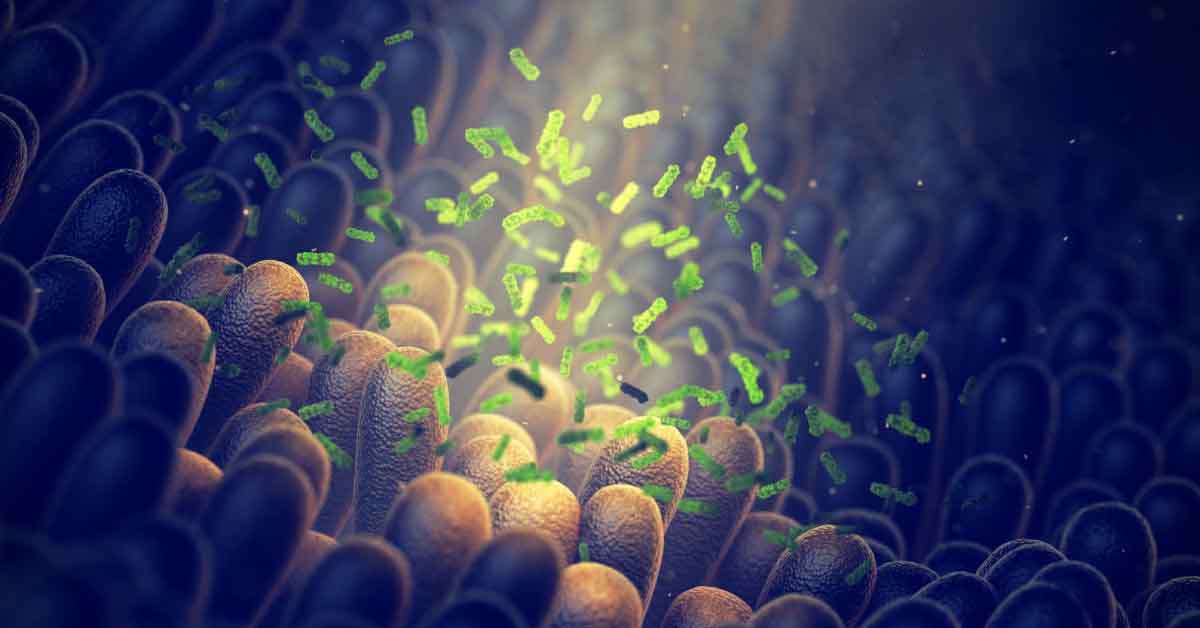
In a healthy digestive system, some of the bacteria comprising the gut microbiome produce metabolites such as butyrate that foster the growth of beneficial bacteria and maintain the lining of the gut. When a person’s microbiome is somehow compromised and lacks these butyrate-producing bacteria, fragments of partially digested food can leak out of the gut and wreak havoc on the immune system causing allergic reactions and other ailments.
One option for treating those with allergies would be to restore the missing bacteria orally or with a fecal transplant, but that hasn’t worked well in the clinic, according to Jeffrey Hubbell, PhD, one of the project’s principal investigators. “So we thought, why don’t we just deliver the metabolites — like butyrate — that a healthy microbiome produces?”
“But butyrate has a very bad smell, like dog poop and rancid butter, and it also tastes bad, so people wouldn’t want to swallow it,” says Shijie Cao, PhD, who will present the results at the meeting for the University of Chicago-based team. And even if people could choke it down, butyrate would be digested before reaching its destination in the lower gut.
To overcome these challenges, the researchers, including principal investigators Cathryn Nagler, PhD, and Ruyi Wang, PhD, designed a new delivery system by polymerizing butanoyloxyethyl methacrylamide — which has a butyrate group as a side chain — with methacrylic acid or hydroxypropyl methacrylamide. The resulting polymers self-assembled into aggregates, or polymeric micelles, that tucked the butyrate side chains in their core, thus cloaking the compound’s foul smell and taste.
The researchers administered these micelles to the digestive systems of mice lacking either healthy gut bacteria or a properly functioning gut lining. After digestive juices released the butyrate in the lower gut, the inert polymers were eliminated in the feces. The treatment restored the gut’s protective barrier and microbiome, in part by increasing the production of peptides that kill off harmful bacteria, which made room for butyrate-producing bacteria.
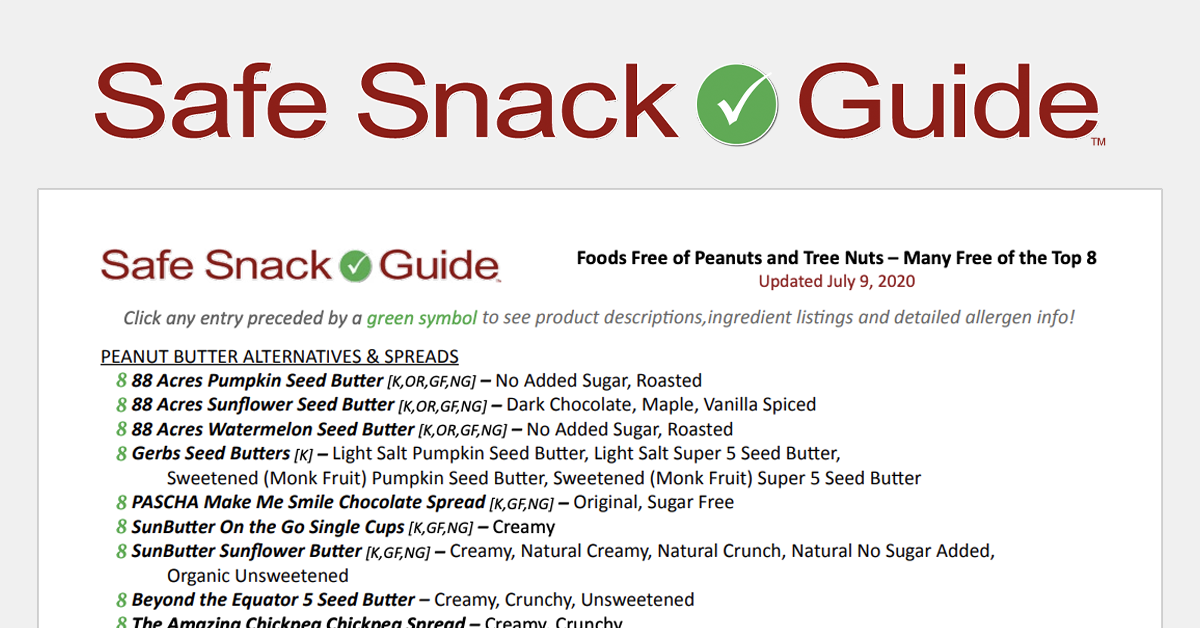
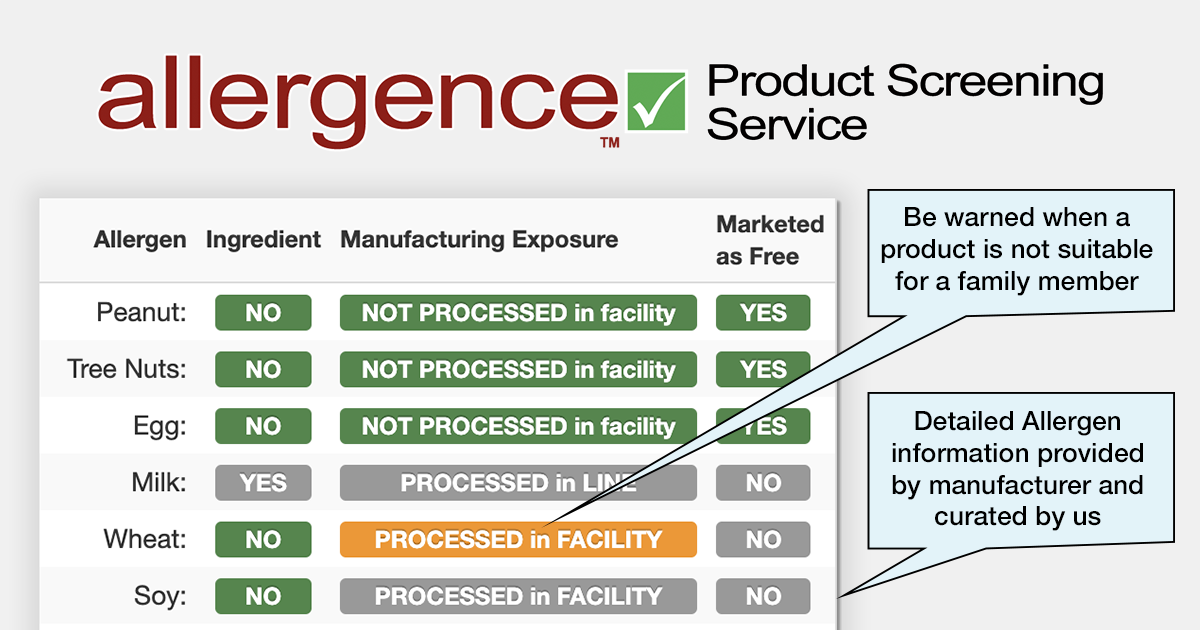
Most importantly, dosing allergic mice with the micelles prevented a life-threatening anaphylactic response when they were exposed to peanuts. “This type of therapy is not antigen-specific,” Cao notes. “So theoretically, it can be broadly applied to any food allergies through the modulation of gut health.”
Next up are trials in larger animals, followed by clinical trials. If those trials succeed and the US Food and Drug Administration approves the oral treatment, the micelles could be marketed in small packets; consumers would tear open a packet and stir the contents into a glass of water or juice. In other work with the micelles, the team is analyzing data on treating inflammatory bowel diseases with the oral therapy.
The team is also investigating administration via injection. The researchers have shown that this method allows the micelles and their butyrate cargo to accumulate in lymph nodes, which are part of the immune system. They found that this approach is effective in treating peanut allergies in mice, but it could also be used to suppress immune activation locally — rather than throughout the body. For example, injections could be helpful in patients who have had an organ transplant or who have a localized autoimmune and inflammatory condition, such as rheumatoid arthritis.
The researchers will present their results at the fall meeting of the American Chemical Society, a meeting held virtually and in person August 21–25.
See the media briefing from the ACS here: