We know that prompt administration of epinephrine as soon as anaphylaxis is suspected leads to better outcomes, but are we using it often enough when our kids react? (Hint: No, we’re not.)
“Predictors for epinephrine undertreatment have been poorly studied,” write Neta Cohen, MD, of the division of pediatric emergency medicine at the University of Toronto, and colleagues.
So Cohen and colleagues reviewed the charts of 368 children (median age, 5.4 years) who presented with anaphylaxis-like symptoms to a busy tertiary care facility emergency department (ED) in Toronto.
They determined that although 90.8% of the children were correctly diagnosed with anaphylaxis, nearly a quarter (23.7%) were not treated with epinephrine. Of those, 13 had full resolution of signs and symptoms during the ED presentation.
According to the researchers, the predictors of patients not receiving epinephrine included those whose reactions occurred at home, those with a first-ever occurrence of anaphylaxis, and those with reactions that started as mild.
The study concluded:
This is the first North American study to explore the rates of correct diagnosis in patients presenting to the pediatric ED with anaphylaxis by using retrospective chart revalidation. Ongoing efforts should be made to promote epinephrine treatment and patient education.
Said Dr Wes Sublett to Healio:
Previous studies that examined patient care before and during ED evaluation for anaphylaxis have demonstrated an underuse of epinephrine by both patients and physicians, the lack of prescriptions and education of epinephrine autoinjectors at ED discharge and a low rate of referral to allergists for follow up. Therefore, Cohen and colleagues’ study, which had similar findings, shows opportunities continue to exist for improving emergency treatment and management of anaphylaxis.
The underutilization of epinephrine in anaphylaxis, despite being first-line treatment, is concerning and shows we have a long way to go in achieving optimal care for anaphylaxis.
ED physicians and other health care professionals can use the National Institute of Allergy and Infectious Diseases/Food Allergy and Anaphylaxis Network, which contains three clinical criteria that identify likely anaphylaxis.
It is important to note that while antihistamines may relieve some anaphylaxis symptoms — such as flushing, urticaria (hives) and angioedema (swelling) — epinephrine is the only first-line treatment for anaphylaxis and should be administered first. A delay in administering epinephrine can cause poor outcomes and death. After treatment, a referral to a board-certified allergist-immunologist is critical to evaluate for potential triggers of anaphylaxis and to provide additional education to patients on the use of epinephrine.
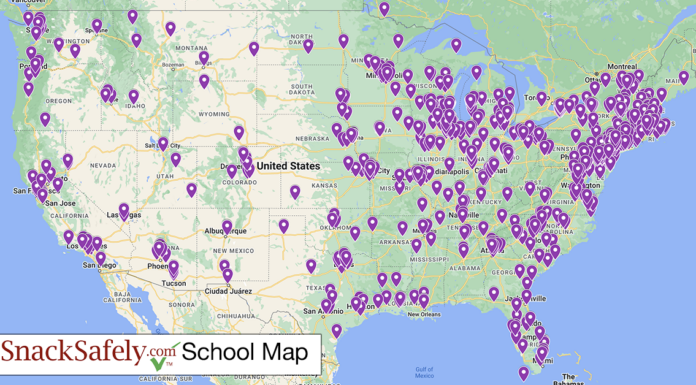
SnackSafely.com has resources to help you prepare for an anaphylactic emergency in your household:
- Epinephrine First, Period makes the case for prompt administration of epinephrine as soon as you suspect anaphylaxis as advised by the American Academy of Pediatricians;
- How to Determine Whether it’s Anaphylaxis provides a quick decision chart developed by Food Allergy Research and Education (FARE) for determining whether the symptoms you see rise to the level of anaphylaxis;
- Know Your Epinephrine Auto-Injector Options and How to Use Your Device provides descriptions and videos showing how each device offered for sale in the US is administered.