Researchers at McMaster University have found another application for an antibody being tested for asthma that could potentially treat food allergies by interrupting the body’s key signaling mechanism during anaphylaxis. Their study was recently published in The Journal of Allergy and Clinical Immunology.
It is understood the immune systems of people with food allergies mistakenly identify a food protein as an invader and develop an antibody known as immunoglobulin E (IgE) to clear it from the body. Once this happens, the immune system retains a “memory” of the allergen and will mount a response whenever it is detected triggering the symptoms of allergic reactions and anaphylaxis. This response involves a complex series of chemical signals that result in the production of IgE.
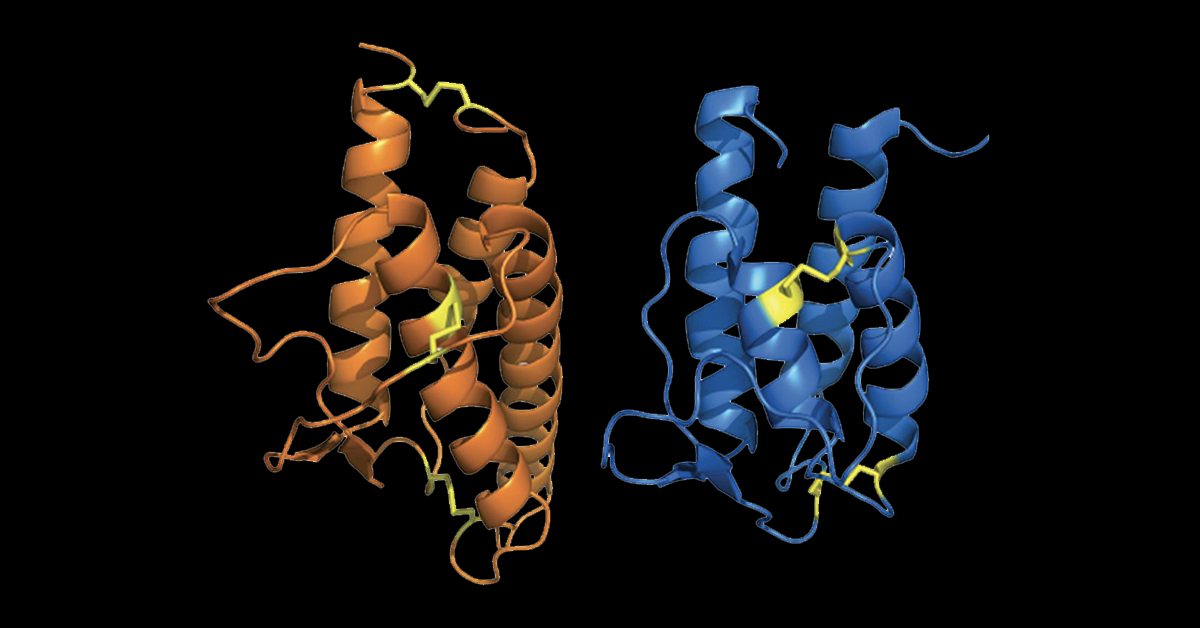
Researchers at McMaster University focused on two of those chemical signals from the interleukin family of proteins, IL-4 and IL-13. They found that by blocking these signaling proteins, the body stopped short of producing IgE, preventing anaphylaxis in mice that were sensitized to peanuts.
“This research suggests a potentially transformative treatment for peanut allergy in particular and food allergies in general,” said Dr Manel Jordana, a member of the McMaster Immunology Research Centre and co-lead author on the study.
“These results spotlight IL-4 receptor blockade as a therapy with disease-transformative potential for the treatment of food allergy and offers new hope for our patients,” said Dr Susan Waserman, professor of medicine and director of the Division of Clinical Immunology and Allergy at McMaster and co-lead author of the study.
The antibody used to block the signaling proteins is being tested to treat asthma, eczema and nasal polyps by Regeneron with clinical trials already underway. The company is looking to expand its potential use to treat food allergies as well.