Anaphylaxis is an acute, life-threatening systemic reaction to a food, drug, insect venom, or environmental factor.
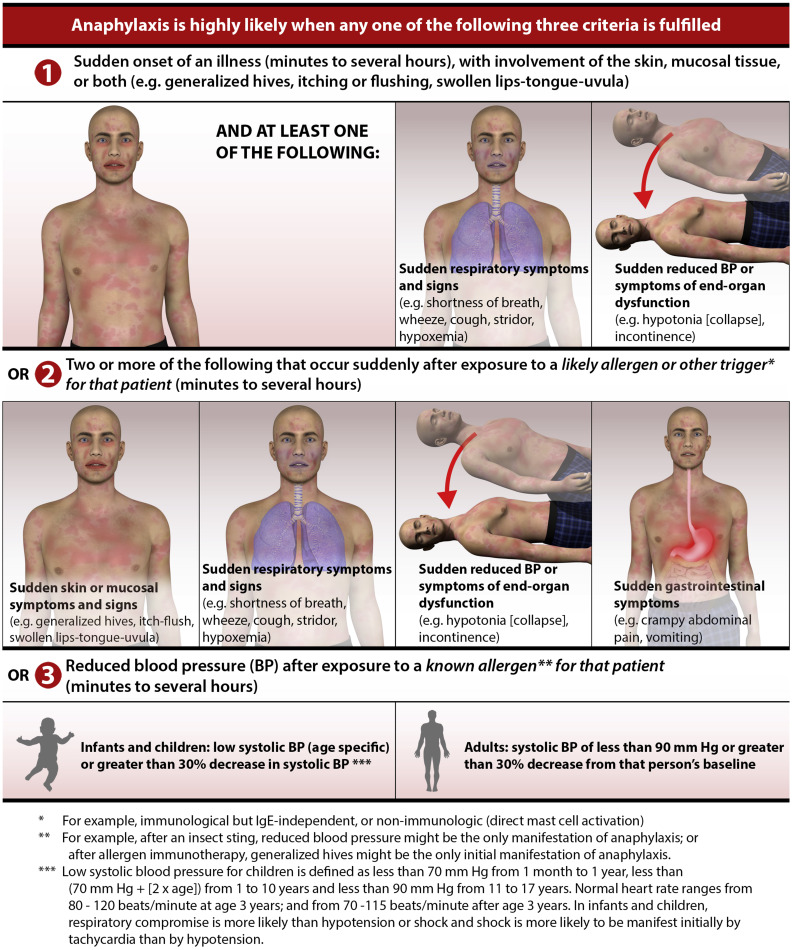
Because anaphylaxis is systemic in nature, it can often present in a multitude of symptoms. A practice update published in April in the Journal of Allergy and Clinical Immunology provides the following graphic to help clinicians diagnose anaphylaxis:
The report makes clear the role and importance of epinephrine as the first-line treatment for anaphylaxis. Here are four “good practice” recommendations highlighted in the report:
Good practice statement 1. Administer epinephrine as the first-line pharmacotherapy for uniphasic and/or biphasic anaphylaxis.
Good practice statement 2. Do not delay the administration of epinephrine for anaphylaxis, as doing so may be associated with higher morbidity and mortality.
Good practice statement 3. After diagnosis and treatment of anaphylaxis, all patients should be kept under observation in a setting capable of managing anaphylaxis until symptoms have fully resolved.
Good practice statement 4. All patients with anaphylaxis should receive education on anaphylaxis, including avoidance of identified triggers, presenting signs and symptoms, biphasic anaphylaxis, treatment with epinephrine, and the use of epinephrine auto-injectors, and they should be referred to an allergist. Of note, there may be some circumstances where self-injectable epinephrine is deferred (ie, resolved anaphylaxis and drug trigger with high likelihood of successful avoidance) and shared decision making may play a role in some circumstances.
Biphasic anaphylaxis is the second onset of symptoms that can occur hours after the initial phase. Little is known about the causes of biphasic anaphylaxis making the identification of patients at risk difficult. Such reactions are estimated to occur in about 5% of patients treated for an initial bout of anaphylaxis and can be serious.
Since a biphasic reaction can occur up to 72 hours after the initial reaction, determining how long to keep a patient under observation after symptoms of the initial reaction resolve is difficult given the paucity of data.
The report indicates that at least one hour of post-symptom observation is warranted for individuals at “low risk” for biphasic reactions, while 6 hours or longer may be needed for those at higher risk. Unfortunately, determining who is at low vs high risk with the information available today is difficult.
In the absence of sufficient clinical data, the authors of the report provide consensus recommendations on a number of risk factors that warrant extended observation (though they indicate the certainty of their recommendations is very low):
Recommendation 1: We suggest that a clinician incorporate severity of anaphylaxis presentation and/or the administration of >1 dose of epinephrine for the treatment of initial anaphylaxis as a guide to determining a patient’s risk for developing biphasic anaphylaxis. Conditional recommendation. Certainty rating of evidence: very low.
Recommendation 2: We suggest extended clinical observation in a setting capable of managing anaphylaxis (to detect a biphasic reaction) for patients with resolved severe anaphylaxis and/or those who need >1 dose of epinephrine. Conditional recommendation. Certainty rating of evidence: very low.
The authors go on to make a recommendation about whether antihistamines and steroids should be administered to prevent a biphasic occurrence:
Recommendation: We suggest against administering glucocorticoids or antihistamines as an intervention to prevent biphasic anaphylaxis. Conditional recommendation. Certainty rating of evidence: very low.
The report goes on to make recommendations for those that suffer anaphylaxis from contrast dyes, chemotherapy, and aeroallergy rush immunotherapy (RIT), all with very low confidence.
Though the tepidness of the authors’ recommendations regarding biphasic reactions is frustrating, keep in mind that they consider the patient at high risk of developing a biphasic reaction if the initial bout of anaphylaxis was determined by the clinician to be “severe” or if more than one administration of epinephrine was necessary to treat the initial bout.
Should you find yourself or a loved one in the hospital being treated for anaphylaxis and your circumstances indicate “high-risk”, be your own advocate and discuss a longer observation time with the physician.
Take the 10-Second Quiz, Then Sign the Petition





