Thanks to a milder winter in many parts of the US, tick season is expected to start earlier, last longer, and present ever more danger of contracting tick-borne diseases.
The list of tick-transmitted disease — the stuff of nightmares — includes Anaplasmosis, Babesiosis, Borrelia mayonii, Borrelia miyamotoi, Bourbon virus, Colorado tick fever, Ehrlichiosis, Heartland virus, Lyme disease, Powassan disease, Rickettsia parkeri, Rocky Mountain spotted fever, STARI (Southern tick-associated rash illness), Tickborne relapsing fever, Tularemia, and 364D rickettsiosis.
Add to that one of the newest nightmares to explode on the scene — Alpha-Gal Syndrome (AGS) — which results in an allergy to red (mammalian) meat and can trigger anaphylaxis.
Last fall, the Centers for Disease Control (CDC) warned the incidence of suspected AGS was rising with the area of suspected cases expanding across much of the US:
Here follows our Q&A to help you protect your family from AGS and other tick-borne diseases this spring.
What is alpha-gal?
Alpha-gal (galactose-α-1,3-galactose) is a sugar molecule found in most mammals. Alpha-gal is not found in fish, reptiles, birds, or people. Alpha-gal can be found in meat (pork, beef, rabbit, lamb, venison, etc.) and products made from mammals (including gelatin, cow’s milk, and milk products). [Source: CDC]
What is alpha-gal syndrome?
Alpha-gal syndrome is a recently identified type of food allergy to red meat. It triggers an immune system reaction that later produces mild to severe allergic reactions when a person with alpha-gal syndrome eats red meat.
Researchers now believe that some people who have frequent, unexplained anaphylactic reactions — and who test negative for other food allergies — may be affected by alpha-gal syndrome. [Source: Mayo Clinic]
What are the symptoms of alpha-gal syndrome?
As with other food allergies, signs or symptoms of an allergy to alpha-gal may include:
- Hives and itching
- Swelling of your lips, face or eyelids
- Shortness of breath, cough or wheezing
- Abdominal pain, nausea, diarrhea or vomiting
The most severe reaction, anaphylaxis, can present as a combination of several of these symptoms, may include low blood pressure, and is potentially fatal.
Because these symptoms are delayed, you may only wake up with them in the middle of the night after an evening meal. [Source: AAAAI]
How is alpha-gal syndrome transmitted?
Alpha-gal is a molecule carried in the saliva of the Lone Star tick and other potential arthropods typically after feeding on mammalian blood. People that are bitten by the tick, especially those that are bitten repeatedly, are at risk of becoming sensitized and producing the IgE necessary to then cause allergic reactions. [Source: AAAAI]

Chigger bites are also suspected to transmit alpha-gal syndrome. [Source: Wake Forest Baptist Medical Center]

The incidence of tick bites is much higher in the southern and eastern US, the traditional habitat for the tick. However, cases are now increasingly reported in the northern and western states. And it is a phenomenon that has been observed worldwide, with different ticks responsible for similar cases of red meat allergy in many other countries such as Sweden, South Africa and Australia. [Source: AAAAI]
What are the triggers of reactions in alpha-gal syndrome?
Symptoms of an alpha-gal allergy commonly appear 3-6 hours after eating meat (e.g., beef, lamb, pork, venison, and rabbit) or exposure to products containing alpha-gal. [Source: CDC]

People with antibodies related to alpha-gal syndrome can have allergic reactions to the cancer drug cetuximab (Erbitux). Cetuximab-induced cases of this condition are most common in regions with a high population of Lone Star ticks, suggesting a possible link between Lone Star tick bites and an increased vulnerability to alpha-gal syndrome. More research is needed to understand the connection between ticks that carry alpha-gal in certain regions and cases of alpha-gal syndrome that don’t seem directly linked to tick bites. [Source: Mayo Clinic]
This list of medications includes antibodies derived from animals, like rattlesnake anti-venom. It also includes products that contain gelatin, like certain vaccines or gel-based products. Heart valves that are harvested from pigs and used to replace a failed valve have also been reported to cause reactions or a more rapid breakdown of the valve in alpha-gal allergic patients. [Source: Vanderbilt University]
How is alpha-gal syndrome diagnosed?
Diagnosis of this allergy starts with your allergist taking an appropriate history and physical examination. Because the onset is usually quite delayed, it can be hard to associate the symptoms with eating red meat many hours previously. Triggers include any red meat – including beef, pork, lamb or even horse products. It may occur after eating hotdogs and hamburgers. In very rare cases the reaction may extend to milk or dairy proteins and gelatin.
Your allergist may recommend testing that includes skin tests to the relevant animal proteins and blood tests that measure the levels of a specific immunoglobulin E (IgE) antibody to mammalian meats. An investigational blood test, IgE against alpha-gal itself, may also aid in the diagnosis. [Source: AAAAI]
How is alpha-gal syndrome treated?
As with any food allergy, alpha-gal syndrome treatment involves avoiding the foods that cause your reaction. Always check the ingredient labels on store-bought foods to make sure they don’t contain red meat or meat-based ingredients. Check soup stock cubes, gravy packages and flavor ingredients in prepackaged products. Ask your doctor or allergist for a list of foods to avoid, including meat extracts used in flavoring. The names of some ingredients make them difficult to recognize as meat based.
Use extra caution when you eat at restaurants and social gatherings. Many people don’t understand the seriousness of an allergic food reaction, and few realize meat allergies even exist and that even a small amount of red meat can cause a severe reaction.
If you are at all worried that a food may contain something you’re allergic to, don’t try it. Come prepared to social events to avoid the risk of exposure. For example, if you’re attending a party where guests prepare food on a shared cooking surface, bring your own pre-cooked food.
For a severe allergic reaction, you may need an emergency injection of epinephrine and a visit to the emergency room. Many people with allergies carry an epinephrine auto-injector (EpiPen, Auvi-Q, others). This device is a syringe and concealed needle that injects a single dose of medication when pressed against the thigh. Once you’ve been diagnosed with alpha-gal syndrome, your doctor or allergist likely will prescribe an epinephrine auto-injector. [Source: Mayo Clinic]
How do I protect myself from developing alpha-gal syndrome?
Before You Go Outdoors
Know where to expect ticks. Ticks live in grassy, brushy, or wooded areas, or even on animals. Spending time outside walking your dog, camping, gardening, or hunting could bring you in close contact with ticks. Many people get ticks in their own yard or neighborhood.
Treat clothing and gear with products containing 0.5% permethrin. Permethrin can be used to treat boots, clothing and camping gear and remain protective through several washings. Alternatively, you can buy permethrin-treated clothing and gear.
Use Environmental Protection Agency (EPA) registered insect repellents containing DEET, picaridin, IR3535, Oil of Lemon Eucalyptus (OLE), para-menthane-diol (PMD), or 2-undecanone. EPA’s helpful search tool can help you find the product that best suits your needs. Always follow product instructions.
- Do not use insect repellent on babies younger than 2 months old.
- Do not use products containing OLE or PMD on children under 3 years old.
Avoid Contact with Ticks
- Avoid wooded and brushy areas with high grass and leaf litter.
- Walk in the center of trails.
After You Come Indoors
Check your clothing for ticks. Ticks may be carried into the house on clothing. Any ticks that are found should be removed. Tumble dry clothes in a dryer on high heat for 10 minutes to kill ticks on dry clothing after you come indoors. If the clothes are damp, additional time may be needed. If the clothes require washing first, hot water is recommended. Cold and medium temperature water will not kill ticks.
Examine gear and pets. Ticks can ride into the home on clothing and pets, then attach to a person later, so carefully examine pets, coats, and daypacks.
Shower soon after being outdoors. Showering within two hours of coming indoors has been shown to reduce your risk of getting Lyme disease and may be effective in reducing the risk of other tickborne diseases. Showering may help wash off unattached ticks and it is a good opportunity to do a tick check.
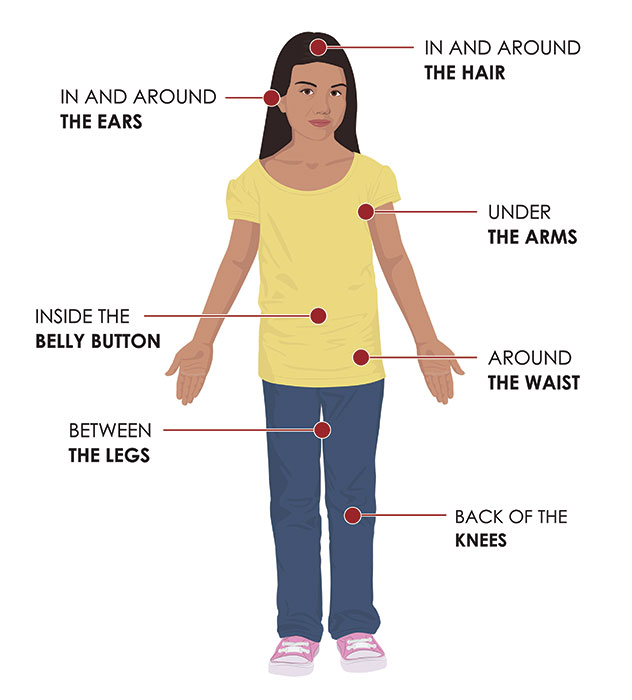
Check your body for ticks after being outdoors. Conduct a full body check upon return from potentially tick-infested areas, including your own backyard. Use a hand-held or full-length mirror to view all parts of your body. Check these parts of your body and your child’s body for ticks:
- Under the arms
- In and around the ears
- Inside belly button
- Back of the knees
- In and around the hair
- Between the legs
- Around the waist
[Source: CDC]
Any observed ticks should be removed carefully by cleaning the site with rubbing alcohol, then using tweezers to pull the tick’s head up carefully from the skin using steady pressure. Clean your hands and the site one more time and make sure not to crush the tick between your fingers. [Source: AAAA]
- Alpha-gal Syndrome — CDC
- Alpha-gal syndrome — Mayo Clinic
- Alpha-gal found to be both a medication and red meat allergy — Vanderbilt University
- Alpha-Gal and Red Meat Allergy — AAAAI
- Allergists Warn that Chigger Bites May Cause Allergic Reaction to Red Meat — Wake Forest Baptist Health